What are dental implants afraid of? Afraid of pathological changes!
"my mother has almost lost all her teeth. I want to give her a dental implant, but I've heard that there will be complications. Is that true?
"what on earth is an implant tooth? Is it safe? "
"I'm so miserable that it takes me more than an hour to eat with dentures, and I still can't feel what I've eaten!"
"the teeth of the old people in the family have been missing for more than a decade. Will there be inflammation after planting teeth?"
At present, implant-supported restoration has gradually become one of the important ways to repair tooth loss. With the continuous improvement of implant retention rate (survival rate) and implant success rate (success rate), oral implant therapy has been widely carried out.
The editor has also heard many friends' doubts and worries about dental implants. of course, implant therapy may also fail because of some biological complications, so today, let's talk about the possible problem of dental implant technology in Ch á ng (hu ball) dental implant technology-peri-implant lesions.
Peri-implant lesion
Peri-implant lesion (lesion of peri-implant), also known as peri-implant tissue inflammation, refers to the inflammatory damage that occurs in the soft and hard tissue around the implant, including peri-implant mucositis involving only soft tissue and periimplant inflammation involving the implant bed and causing significant bone resorption. If the latter is not treated in time, it will lead to continuous bone resorption and "disintegration" (disintegration) of the implant-bone interface, resulting in implant loosening and shedding. Periodontitis is one of the main reasons that affect the long-term effect of dental implant and lead to implant failure.

Pathogeny
Smoking: smoking has been confirmed to be one of the major risk factors for periodontitis and peri-implant periodontitis. Data show that the incidence of peri-implant inflammation in smokers (9.2%) is higher than that in non-smokers (5.3%).
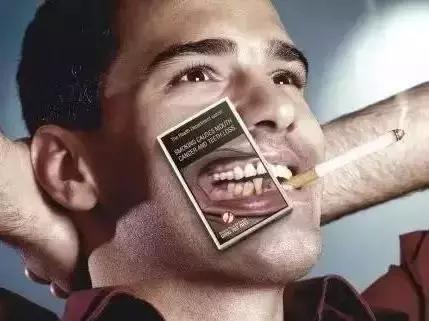
Tobacco contains a lot of toxic substances, among which nicotine has been proved to have a strong vasoconstriction, which will affect the blood supply and the transport of nutrients. In addition, smoking can change the oral environment around various implants, reduce the healthy flora around the implant and increase the accumulation of pathogens around the implant.
Therefore, for patients with dental implant plans, we usually advise them to quit smoking or reduce smoking.
Plaque: plaque accumulation is an important factor leading to peri-implant inflammation. Healthy implants are mainly surrounded by aerobic or facultative anaerobic cocci or bacilli. When there is inflammatory damage around the implant, it is mainly surrounded by gram-negative anaerobes, including a large number of active bacilli, clostridium and spirochetes.
Do you understand me? Neither did I.
However, the doctor told the editor that oral hygiene must be paid attention to after dental implants. Get into the habit of brushing your teeth and gargling after meals every morning and evening. If we do not pay attention to oral hygiene, long-term retention of food residue will cause the accumulation of plaque, and the reproduction of plaque will cause biological damage to the junction of gingiva and implant, thus causing peri-implant inflammation to shorten the life of dental implants.
Biomechanical overload: overocclusal load is an important driving factor in the pathogenesis of peri-implant inflammation. In other words, problems such as abnormal occlusal relationship, poor retention of dentures, inappropriate number of implants, problems in denture design, incorrect position of implants, abnormal relationship between upper and lower jaw, and so on, may lead to peri-implant inflammation.
clinical manifestation
The clinical manifestation of peri-implant periodontitis is similar to periodontitis, which is asymptomatic in the early stage and is usually found on reexamination.
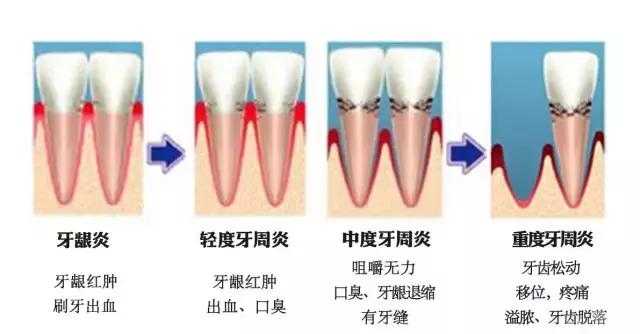
The typical clinical manifestations of peri-implant inflammation are: redness and swelling of mucosa, bleeding on probing, empyema in the peri-implant pocket, increased depth of probing and decrease of osseointegration. X-ray examination showed various types of bone resorption and typical symmetrical "shallow disc" (or "bullet pit") bone defect.
- Prev

Experience | key points for planting potted lilies
Key points of potted lily planting every year there will be lily producers who do not use cold storage to take root, resulting in products that are too short and buds too small to sell.
- Next

How much do you know about dental implants?
The invention of dental implants took place in 1952, an epoch-making event in the history of dental implants. At a university called University of Lund in Sweden.
Related
- Fuxing push coffee new agricultural production and marketing class: lack of small-scale processing plants
- Jujube rice field leisure farm deep ploughing Yilan for five years to create a space for organic food and play
- Nongyu Farm-A trial of organic papaya for brave women with advanced technology
- Four points for attention in the prevention and control of diseases and insect pests of edible fungi
- How to add nutrient solution to Edible Fungi
- Is there any good way to control edible fungus mites?
- Open Inoculation Technology of Edible Fungi
- Is there any clever way to use fertilizer for edible fungus in winter?
- What agents are used to kill the pathogens of edible fungi in the mushroom shed?
- Rapid drying of Edible Fungi

